Blood glucose homeostasis is vital for metabolic health. Chronic dysregulation leads to insulin resistance, β-cell dysfunction, and diabetes mellitus. Hemoglobin A1c (HbA1c) is a robust biomarker reflecting long-term glycemic exposure and is strongly associated with metabolic complications. This article outlines the physiological regulation of blood glucose, the biochemical basis of HbA1c, and its clinical relevance.
1. Physiology of Blood Glucose Regulation
Glucose serves as the primary cellular energy source and is regulated through a balance of dietary intake, hepatic glucose production, and peripheral uptake. Insulin, secreted by pancreatic β-cells, facilitates glucose uptake in muscle and adipose tissue via GLUT-4 translocation and suppresses hepatic gluconeogenesis. Counter-regulatory hormones—glucagon, cortisol, catecholamines, and growth hormone—raise blood glucose during fasting or stress. Normal fasting glucose is maintained between 70–99 mg/dL.
2. Pathophysiology of Hyperglycemia
Insulin resistance reduces cellular responsiveness to insulin, leading to compensatory hyperinsulinemia and eventual β-cell exhaustion. Persistent hyperglycemia activates pathogenic pathways, including formation of advanced glycation end products (AGEs), increased oxidative stress, mitochondrial dysfunction, and chronic inflammation. These mechanisms contribute to endothelial injury and progressive organ damage.
3. Biochemical Basis of HbA1c
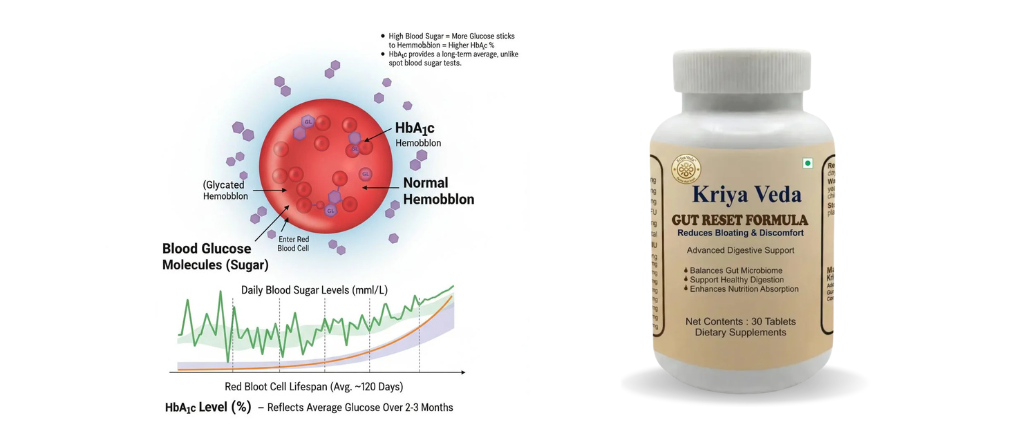
HbA1c is formed by non-enzymatic glycation of hemoglobin when circulating glucose binds to hemoglobin β-chains within erythrocytes. Since red blood cells have a lifespan of approximately 120 days, HbA1c reflects mean blood glucose over the previous 8–12 weeks. Higher glucose exposure proportionally increases HbA1c levels.
4. Clinical Interpretation and Significance
HbA1c (%) Interpretation
< 5.7 Normal
5.7–6.4 Prediabetes
≥ 6.5 Diabetes
Each 1% rise in HbA1c corresponds to an approximate 30 mg/dL increase in average plasma glucose. HbA1c is a strong predictor of microvascular and macrovascular complications.
5. Limitations and Influencing Factors
HbA1c accuracy may be affected by altered erythrocyte turnover, anemia, hemoglobinopathies, chronic kidney disease, and iron deficiency. Therefore, HbA1c should be interpreted alongside fasting and postprandial glucose measurements.


